Coagulation and Cancer
The Relationship between Clotting and Cancer
Introduction
According to WHO, the top ten global causes of death are led by ischemic heart disease and strokes. Various studies have proved that solid tumours and haematological malignancies have different causes leading to a stroke.
A stroke is one of the primary detection criteria for cancer and its mechanism is directly related to coagulation disorders, infections, and therapy. It has been well documented and studied that a stroke occurs more frequently in cancer patients as compared to the average population(1).
A malignant tumor may affect the hemostatic system that leads to a number of coagulation abnormalities in both thrombosis and a hemorrhage disorder. It has been recently proved that thrombotic events complicated haematological malignancies. Acute leukemia, hemorrhage and uncompensated Disseminated Intravascular Coagulation (DIC) complicate the hemostatic condition and can be fatal(2).
Patients receiving active therapy for malignancy may suffer from thromboembolism. These thromboembolic events are of two types:
- Venous Thromboembolism (VTE): Deep Vein Thrombosis (DVT), Pulmonary Embolism (PE) together categorized as Venous Thromboembolism (VTE). (Figure 1)
- Arterial thromboembolism: It includes stroke, and myocardial infarction. (Figure 2). During thromboembolic events, patients may suffer from the following consequences:
- Requirement for long-term anticoagulation
- Risk of bleeding complications
- Recurrent VTE
- Potential impact on chemotherapy delivery
These consequences collectively may affect the quality of life of the patient. Due to these complications thrombotic events are the leading cause of death in cancer patients, and are linked with decreased short-term and long-term survival. VTE consumes a significant amount of healthcare resources to manage malignancy(3).
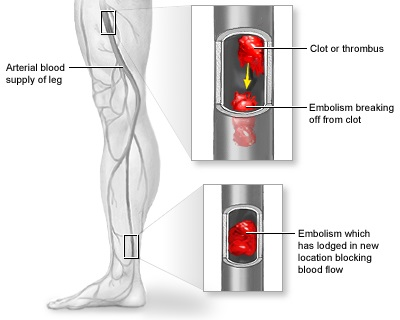 Figure 2: Arterial thromboembolism
Figure 2: Arterial thromboembolism
(Source: https://medlineplus.gov/ency/article/001102.html)
Clinical risk factors for VTE can be categorized as follows:
Patient associated risk factors: This includes older age, race or ethnicity, presence of comorbid conditions, obesity and prior history of thrombosis.
- Cancer associated risk factors: The primary site of cancer is an important risk factor, with highest rates observed in patients with brain, pancreas, stomach, kidney, ovary and lung cancers. Patients with hematologic malignancies are at high risk. The rate of VTE varies during the natural history of the malignancy.
- Treatment associated risk factors: Therapeutic interventions may increase the risk of VTE in cancer and surgeries in cancer treatment further enhance the risk. Hospitalization and systemic chemotherapy may increase risk of VTE compared to the general population. Thalidomide, Lenolidomide, Dexamethasone or Chemotherapy, Bevacizumab, Sunitinib, Sorafenib are therapies which substantially affect the various physiological pathways and may enhance the risk of VTE as well as an arterial thromboembolic event.
A variety of biomarkers are widely used for predicting VTE; few of them are listed below:
- Baseline (pre-chemotherapy) elevated platelet and leukocyte counts
- Low hemoglobin levels
- Components of the complete blood count
- D-dimer
- Tissue Factor (TF), the physiologic initiator of hemostasis.
Various risk assessment tools can be used to identify risk in patients or study population. These risk assessment tools are based on expert consensus and need to be validated properly for use in cancer patients.
(ECL Note: ECL series has entire array of D Dimer testing. Its starts with Erba D Dimer Calibrator (EHL00018), Erba D Dimer Control N + P) (EHL00019), and Erba D Dimer R (EHL00011))
References
- Grisold W, Oberndorfer S, Struhal W. Stroke and cancer: a review. Acta Neurol Scand 2009: 119: 1–16
- Falanga A, Marchetti M, Vignoli A. Coagulation and cancer: biological and clinical aspects. J Thromb Haemost 2013; 11: 223–33
- Alok Khorana; Cancer and Coagulation; Am J Hematol. 2012 May ; 87(Suppl 1): S82–S87.